OVERVIEW
Cultural competence requires an awareness of cultural diversity and the ability to function effectively and respectfully when working with and treating people of different cultural backgrounds. Cultural competence means a healthcare professional has the attitudes, skills and knowledge needed to achieve this.
What is cultural competence?
All health professionals are expected to provide culturally competent care to people and their whānau or families, yet cultural competence is a complex idea to understand. Understanding of what it means has evolved over time.
Initially, cultural competence was presented as a checklist of what the health professional should do if they were working with a person from a different culture, eg, a Pakeha nurse working with a Māori person.
However, nowadays people understand that cultural competence is much more complex than a checklist.
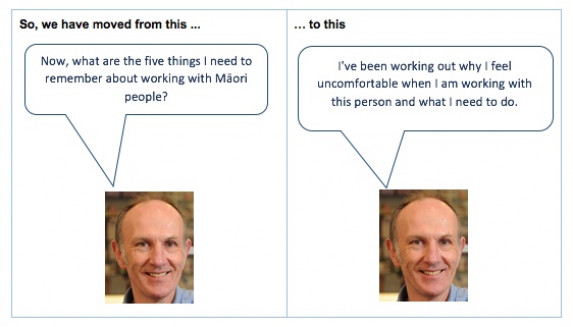
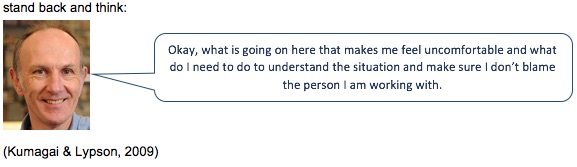
Now cultural competence is recognised as being about the self-awareness, attitudes, skills and knowledge of the health professional. This requires the health professional noticing when they feel uncomfortable or uncertain in a situation and realising that means they need to understand what is inside them that is making them uncomfortable, rather than thinking the other person is the problem.
Researchers have described cultural competence as meaning the health professional and health coach have to understand:
- what assumptions they are making about the situation they are in and the person they are working with
- their own beliefs and biases that are making them feel so uncomfortable
- what is really going on for the person they are working with.
Definitions of cultural competence
Mauri Ora defines cultural competence in the following way:
“Individual values, beliefs and behaviours about health and wellbeing are shaped by various factors such as race, ethnicity, nationality, language, gender, socioeconomic status, physical and mental ability, sexual orientation and occupation. Cultural competence in healthcare is broadly defined as the ability of health practitioners to understand and integrate these factors into the delivery of healthcare practice.”
Another definition that attempts to capture this more contemporary complex understanding of cultural competence comes from the Medical Council of New Zealand:
“Cultural competence requires an awareness of cultural diversity and the ability to function effectively, and respectfully, when working with and treating people of different cultural backgrounds. Cultural competence means a doctor has the attitudes, skills and knowledge needed to achieve this. A culturally competent doctor will acknowledge:
- that New Zealand has a culturally diverse population
- that a doctor’s culture and belief systems influence his or her interactions with patients and accepts this may impact on the doctor-patient relationship.
- that a positive patient outcome is achieved when a doctor and patient have mutual respect and understanding.”
What cultural competence isn’t
Sometimes it is easier to say what cultural competence is not.
| Not cultural competence | Reasons |
| Treating everyone the same | People are never the same, even if they are all Māori, Samoan or Pakeha. In fact, treating everyone the same can make health problems worse, not better. |
| A checklist | There is no list of things to do when you visit a Māori whānau. |
| Learning about other cultures
|
This encourages assumptions, as health professionals say they can know about their own culture as well as other cultures. |
| Coming from the same ethnic group | Just because the health professional and the person they are dealing with are both Māori is no guarantee that the health professional will give culturally competent care. |
| Speaking the same first language | The health professional and the person they are working with might both be speaking English but that is no guarantee that the person will get culturally competent care. |
| Using words that suggest the person is to blame eg, non-adherent, non-compliance, at risk | Using these sorts of words means we have automatically blamed the person rather than tried to understand all the reasons the person is not taking their medicines eg, money, side effects. |
Implicit or unconscious bias
A bias is when you are prejudiced against a person or group in a way that is unfair.
From the time we are born, we learn and take on beliefs and values about the world. We get most of our beliefs and values from our family, friends and the media. If you believe that the Treaty of Waitangi happened a long time ago and should not affect what happens today, then you won’t be in favour of Treaty settlements, Māori seats in Parliament, Māori land rights and Māori rights over water.
Even well-meaning people who do not think of themselves as being racist have these unconscious biases as part of their upbringing.
Understanding your unconscious bias is a really important part of cultural competence. It is your unconscious biases that make you feel uncomfortable in new or unfamiliar situations. If you understand that, you will be more able to feel uncomfortable and not react badly.
Your unconscious biases act like shortcuts and affect your thinking and actions, especially in situations:
- where there are time pressures
- where there are not enough resources
- where there is not enough information
- that need high levels of critical thinking.
Why is cultural competence important?
Because culture impacts on care, health professionals need to be aware of cultural diversity and learn to function effectively and respectfully when working with and treating people of different cultural backgrounds.
Cultural competence helps to address the inequities (lack of fairness) in the healthcare system. For example, there is a lot of information that Māori and Pasifika peoples have much worse health outcomes than other population groups, especially Pakeha. So cultural competence is one way of addressing those inequities (unfairness) that are caused by:
- the design of the health system
- prejudice by healthcare providers and healthcare professionals, eg, beliefs that different groups are not as able, motivated or keen to be as healthy as other groups, such as Pākehā
- discrimination by healthcare providers and healthcare professionals, eg, actions such as not referring Māori people to rehabilitation programmes.
Learn more
Statement on cultural competence New Zealand Medical Council
Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition International Journal for Equity in Health
References
Foundation course in cultural competency Mauri Ora
Building cultural competence – the Medical Council’s direction BPAC, NZ, 2011
RESOURCES
Cultural competence
RNZCGP, NZ, 2
Foundations in Cultural Competency (2016) – LEARN ONLINE COURSE



